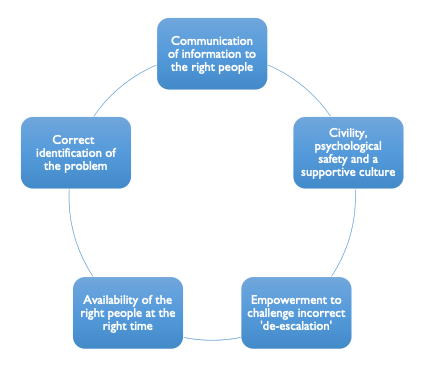
Successful clinical escalation is a complex process that requires a combination of clinical, behavioural and logistical steps in order to correctly identify and deliver urgent care.
In the analysis of Each Baby Counts babies born in 2017, at least one reviewer felt that ‘failure to escalate/act upon risk/transfer appropriately’ occurred in 36% (358/986) of reports.
This was considered to be as a result of either a lack of awareness of deterioration and the need to escalate, or a breakdown in the process of attempted escalation.
Underlying themes were human factors and behaviour, workload and workforce challenges, and errors in communication methods.
Key learning points from the report included:
1. Cognitive biases
Escalation begins with correctly identifying an evolving pathology or a potentially critical situation. Mistakes evaluating and interpreting information may interfere with that assessment and result in missed opportunities to provide timely care.
2. Loss of situational awareness
Intrapartum care is a high-risk environment for loss of situational awareness. Understanding when it is lost and how to minimise risk is essential to maintaining safety.
3. Multidisciplinary team dynamics
Unbalanced skill sets within an unfamiliar team can result in problems identifying the need for escalation and a lack of assertiveness in executing the process.
4. Challenging a decision
All members of the multidisciplinary team must feel empowered to challenge a decision that they feel is incorrect. Where there is disagreement, a third party should be called to provide another opinion and fresh perspective.
5. Timely obstetric reviews
If an urgent medical review is needed and the on-site obstetric team is unable to deliver care in the required time frame, the consultant must be informed and asked to attend.
6. Handover
Loss of escalation momentum can occur owing to incomplete transfer of information between staff. A high-quality handover is essential for continuity of care and for maintaining situational awareness of the unit as a whole.
The EBC L&S interventions directly address points 3 to 6, as well as promoting a flattened hierarchy and psychological safety so that staff can speak up if another member of the team is making a mistake due to a cognitive bias or lack of situational awareness.
