What are behaviours?
Behaviours can be defined as “anything a person does (or does not do) in response to internal or external events”. At the heart of any service improvement is the ability to change the way health care professionals’ practice and work with each other. Health professionals are trained in knowledge and skills to perform clinical practices. However, just because people can do something, this doesn’t mean they will always do it, despite the best intentions. Learning from behavioural science helps us to understand why health professionals behave the way they do and how to enable changes and adoption of new practices using tried and tested tools.
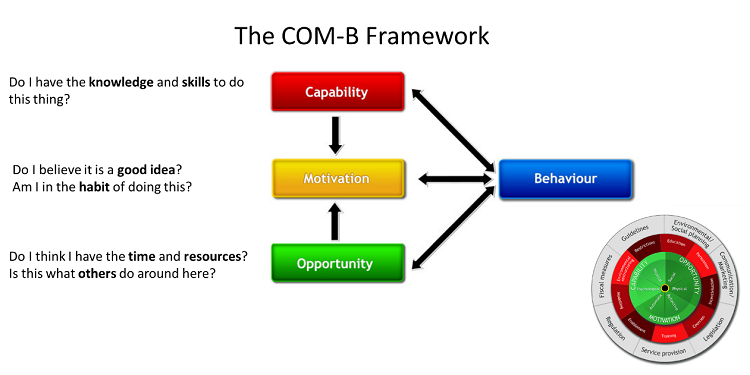
One widely used behavioural science framework is the COM-B model (Michie et al 2011), a comprehensive behavioural science framework that combines many theories and models of behaviour change. According to this framework, in order to change practice, healthcare staff must perceive that they have the capability (knowledge and skills), opportunity (sufficient time, resources and social support) and motivation (including habit) to change. Once we know what drives behaviour, we can use a structured approach to change it.
Watch this animation to learn more about health professional behaviour change:
https://www.mcrimpsci.org/elearningresources/healthcare-professional-behaviour/#toggle-id-2
How to apply a behavioural approach to quality improvement in maternity
A structured behavioural approach to QI involves:
- Understanding what needs to change (behavioural diagnostics) to improve practice in maternity units
- Identify the barriers and facilitators of the practices we want to change or introduce in our unit in terms of capability, opportunity and motivation
- Design and implement intervention strategies to overcome barriers to enable change
- Evaluate the impact of the interventions in practice. Were the new practices adopted by staff? Did they make a different to practice? Were they acceptable and feasible to implement?
Using a structured behavioural approach, we can design impactful interventions that empower teams to overcome barriers to change, and bridge the policy-practice gap by clearly defining the changes teams need to make on a daily basis in concrete and measurable terms. This is the approach we used in Each Baby Counts Learn & Support to improve clinical escalation. Read how we applied the behavioural approach.
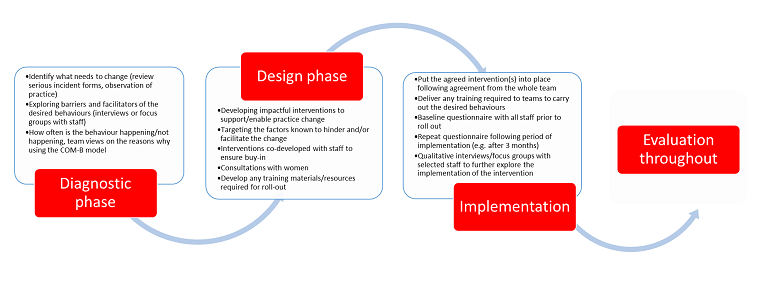
Step 1: Diagnostic phase
Understanding what needs to change and identifying barriers and facilitators
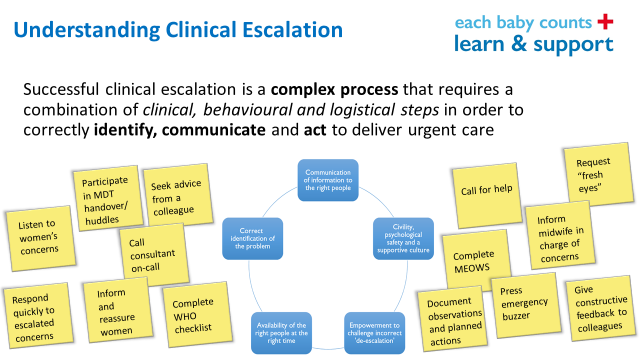
The primary aim of the diagnostic phase is to create a deep understanding of the practice(s) we want to change, alongside the barriers and facilitators. This allows us to tailor our interventions and ensure key barriers are addressed in order to maximise the chances of success. It is important to define who needs to do what differently in order to see any meaningful changes in practice. In our clinical escalation work, we started by unpicking and listing the different practices that can be counted as clinical escalation. As shown below, this identified that clinical escalation is quite complex and often requires multiple actions by different members of the team. Conceptualising clinical escalation in this way allowed us to focus our interventions on three key components of identify, communicate and act. This went onto become our campaign strapline.
Exploring multidisciplinary team members’ views of their capability, opportunity and motivation towards the desired behaviours and practices is really valuable to understanding different perspectives and building early engagement with frontline staff. Also, observing a few shifts on different days and times helps establish how often the behaviours we want to change/introduce are occurring in practice as well as shed further light on the barriers staff may be facing.
See the multi-method diagnostics protocol followed by the Each Baby Counts Learn & Support Leads.
Activities to include your local diagnostics include:
- Consultations/focus groups with staff to understand the barriers and facilitators they encountered
- Consultations/focus groups with women understand the barriers and facilitators they encountered
- Structured observations of practice to establish what needs to change, who needs to do what differently, what are the observed barriers, where are the delays
- Review of local serious incident reports to identify the relevant contributory factors in serious incidents
Learn more about the findings from our Each Baby Counts Learn & Support diagnostics work.
Step 2: Design Phase
In the design phase, we use the learning from the diagnostics to design impactful intervention solutions that address the barriers identified as well as incorporate the factors that help facilitate change. Involving multidisciplinary team colleagues in the design process can be a powerful way of empowering, getting buy-in and engagement with the intervention solutions. Including the perspectives of women, birthing people and their families in the design phase is also good practice and ensures any interventions developed meet their needs.
During the intervention design phase, decisions about how many changes to implement and consensus on what to prioritise for implementation may be required. Factors to consider when making such decisions include the context, complexity and timing of the interventions. Following the EAST (Easy, Accessible, Simple and Timely) approach in intervention design can help with adoption and acceptability from staff. During the design phase, it is also helpful to check whether anyone has implemented something similar locally, nationally or in research publications, and what lessons we can learn from any examples identified.
At this stage, also think about what tools and resources you will need to launch your chosen intervention and prepare these in time for the launch e.g. training slides, posters, logos, emails.
See our slides on how to set up a successful campaign (PPTX 359kb)
Alongside the design of the intervention solutions and materials, think about how you will measure and their evaluate impact. Being able to demonstrate change can also be a powerful way of sustaining it long-term. You may wish to survey staff before and after launching the intervention and/or gather feedback via focus groups.
See our section on evaluation and example measures we used in our Each Baby Counts Learn & Support work.
Step 3: Implementation phase
How-to guide: Successfully launching the interventions
In this phase, the designed interventions are put into practice. Incorporating tried and tested ‘behaviour change techniques’ from behavioural science can aid the adoption of interventions in practice. Behaviour change techniques are the ‘active ingredients’ of change in interventions. Behavioural scientists have produced a taxonomy of 93 behaviour change techniques found to be effective in interventions aiming to change behaviour (Michie et al 2013).
Some relevant behaviour change techniques could include:
- Having a credible source such as head of department introduce the new change
- Information about consequences – tell staff why it is important to address a particular practice/behaviour, what is the impact of this practice being done e.g. positive outcomes for women and babies
- Adding prompts or cues in the environment to remind staff in practice e.g. posters, stickers, business cards
- Social support for staff to reassure and encourage use of the interventions and associated tools
- Problem solving – explicitly probe problems with teams and solutions to overcome them together
- Feedback on behaviour – “this week we had x number of escalations, x babies had a good outcome”. This can help set social norms and establish the accepted standard of behaviour within teams
