Background to the interventions
There are multiple systems in place in maternity settings to recognise deterioration and the need to escalate, but there are very few structured approaches to standardise the behavioural and communication aspects of effective clinical escalation.
Addressing these can therefore positively impact on maternity unit culture, as improving clinical escalation requires solutions to flatten hierarchies, provide psychologically safe working environments, promote optimal teamwork, and support staff.
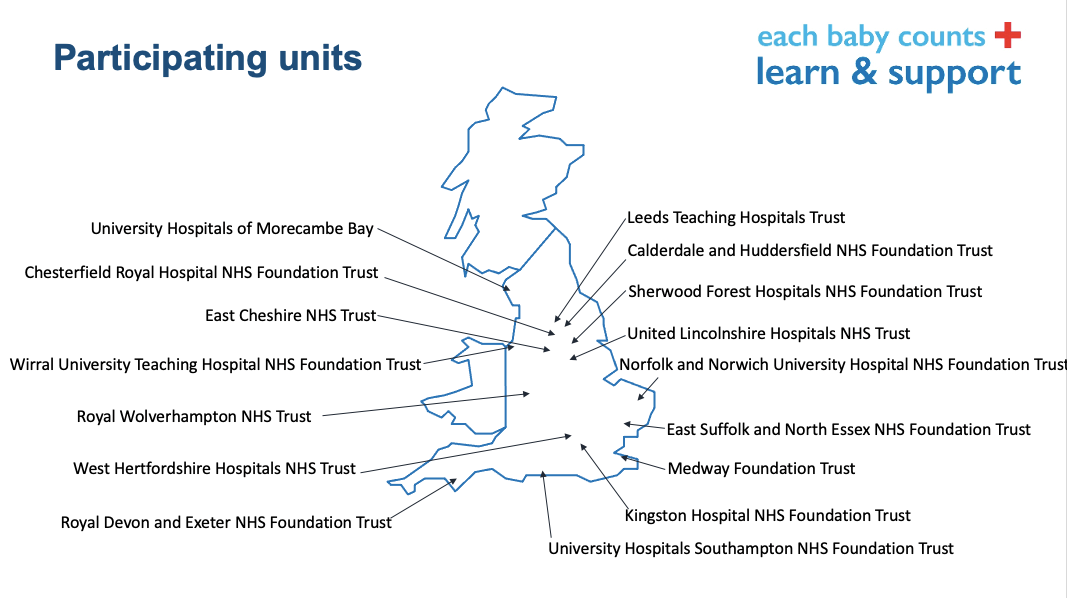
16 maternity departments around the country participated in the programme, each with a designated “local development lead” – a senior midwife or obstetrician working in that hospital.
The units covered all parts of England and included teaching hospitals, district generals, rural, and urban centres.
Find out more about the participating centres, programme team and Local Development Leads (LDLs).
Initially the leads undertook comprehensive “diagnostics” to do a deep dive into the cultural practices of their units and understand what really happens on the shop floor.
Collectively, and co-produced with other maternity staff and service users, they then created solutions to the barriers to effective clinical escalation they had witnessed. This bottom up approach enabled the programme to design interventions that really work, thanks to the ideas, buy in, and enthusiasm of midwives and doctors of all levels.
Three interventions were trialled in the 16 units, with some local adaptation based on existing practices. Using a structured quality improvement approach including comprehensive feedback from staff, they were then refined and developed into the tools contained within this toolkit. Together they formed part of an overarching “campaign” to improve clinical escalation.
The interventions were:
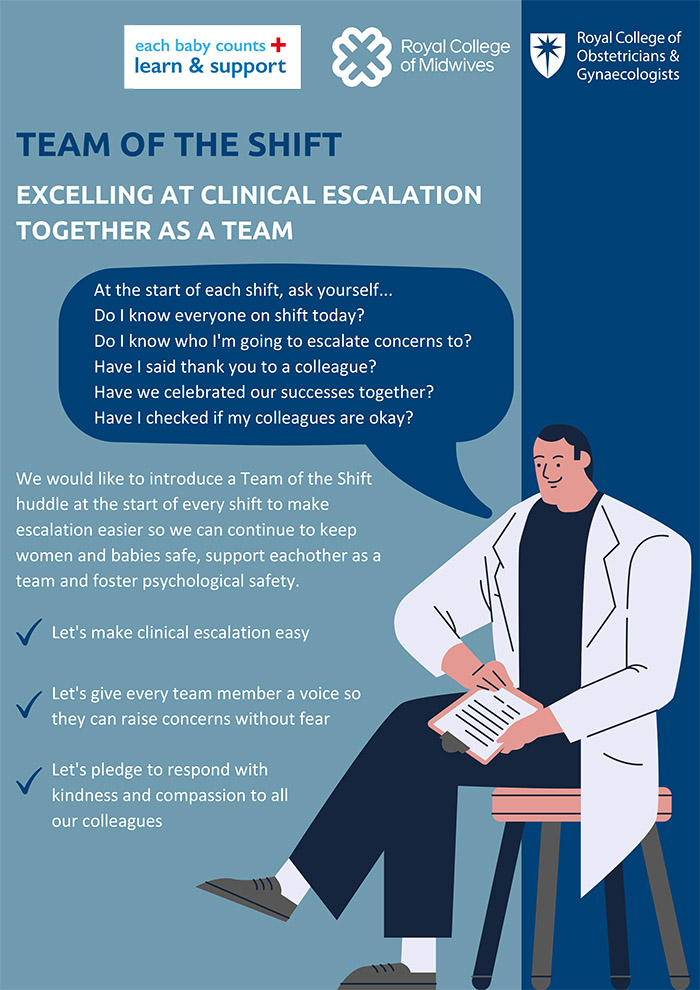
- Team of the Shift – promoting excellence in teamwork
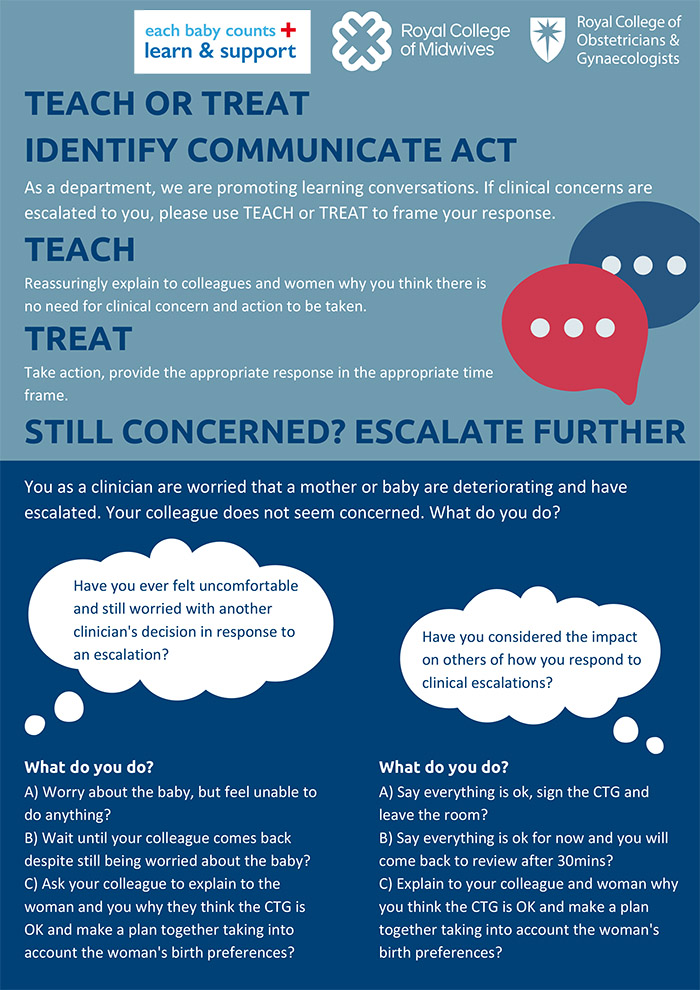
- Teach or Treat – promoting better conversations
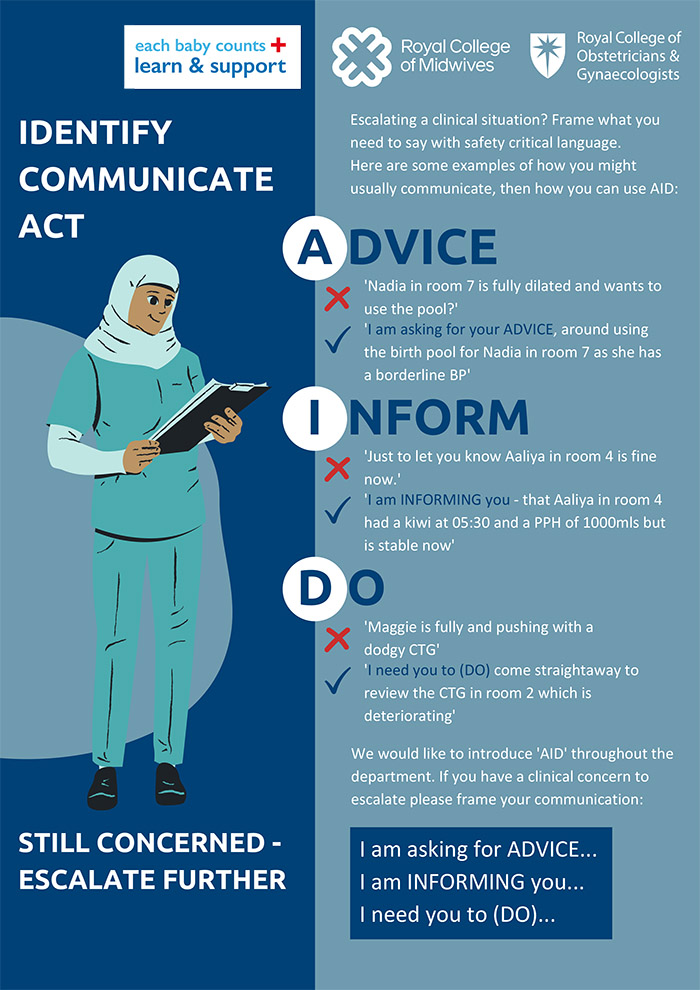
- Advice Inform Do (AID) – safety critical language for escalation
They work alongside and complement “track and trigger” tools such as MEWS, as well as existing communication tools like SBAR. They are simple but effective ways to structure conversations between all healthcare professionals working in maternity settings and promote positive workplace cultures and patient safety.
Downloadable PDF posters from the Escalation toolkit:
Background to the programme
The programme was funded by the Department of Health and Social Care and ran between 2019 and 2022. At the outset, its aims were to work with a network and community of maternity staff, known as Local Development Leads (LDLs), from 16 NHS trusts to:
- Build the capacity of 16 NHS maternity professionals in clinical leadership, safety thinking and quality improvement
- Facilitate of a structured quality improvement process using behavioural science to improve clinical escalation in intrapartum settings
- Evaluate the programme’s training and development approach and the impact of the specific co-designed intervention strategies on clinical escalation.
The LDLs worked together to co-produce, develop and test new approaches to improve the safety and quality of care that focus on behaviours, team work, safety and a positive work culture around clinical escalation.
The programme has three main outputs:
- A final report outlining the findings from the evaluation of the EBC L&S programme in terms of:
- the training and development of LDLs
- LDLs’ experiences and insights of implementation of the quality improvement process in their units, and lessons learnt from applying the behavioural approach to improving clinical escalation
- A refined version of the L&S programme (contained within these webpages)
- A clinical escalation toolkit (contained within these webpages) incorporating the intervention strategies developed and tested that can be rolled out in any maternity unit in the country.