1. Redeployment of O&G staff
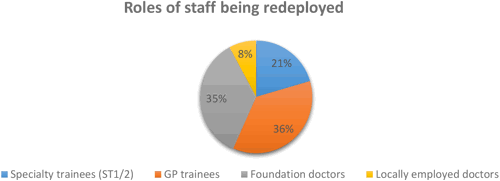
During the COVID-19 pandemic there was significant redeployment of medical staff. 53% of our survey respondents reported that junior grade doctors, including locally employed doctors (LED’s) were redeployed outside of maternity services without reference to specialty requirements. Although the bulk of the redeployment was felt by GP doctors (36%) and foundation doctors (35%), a considerable proportion of O&G specialty trainees (ST1/2) and locally employed doctors were redeployed away from maternity services.
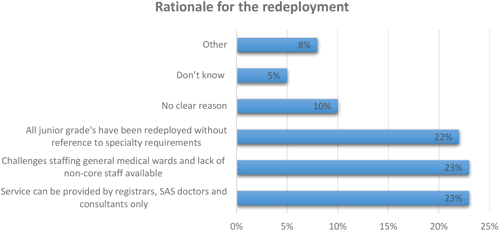
The rationale for the redeployment of junior grade trainees and LED’s was mixed, with 23% of trusts/units reporting that the major challenges in staffing general medical wards, as well as the viewpoint that the maternity services could be delivered by registrars, SAS doctors and consultants, were provided as the primary reasons for the redeployment of these groups. Worryingly, 22% of trusts reported that all junior grade doctors had been redeployed without reference to specialty requirements. 10% of all survey respondents didn’t feel there was a clear reason for the deployment and an additional 5% didn’t understand the rationale for the staffing changes in their trust.
Only 6% of trusts/units confirmed redeployment of middle grade staff (ST3-7) and LED’s outside of the maternity services during the crisis. Similarly, consultants and SAS doctors were also far less likely (7%) than junior grades and LED’s to be redeployed outside of the maternity services.
2. Cover for junior grades and LED’s
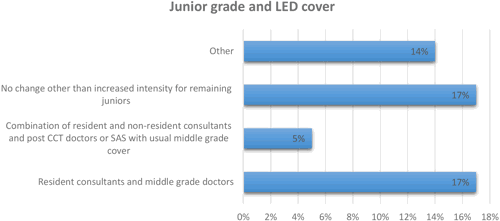
With a considerable proportion of junior grade and locally employed doctors being redeployed, cover was being provided for the most part by resident O&G consultants, SAS and middle grade doctors. 17% of trusts/units reported that there were no changes in cover and remaining junior doctors were working in a more intense way as a result of the redeployment of their colleagues. Only 5% of trusts/units reported that cover was being provided by a combination of resident and non-resident consultants, post CCT and SAS doctors.
3. Redeployment of O&G consultants
Approximately 53% of trusts/units confirmed that O&G consultants and SAS doctors were redeployed to improve obstetric cover for obstetric services instead of gynaecology. 76% of O&G consultants and SAS doctors took on additional caesarean section lists, 60% covered labour wards, 43% re-joined the out of hours’ rota for obstetrics and 30% provided shift cover in antenatal clinics.
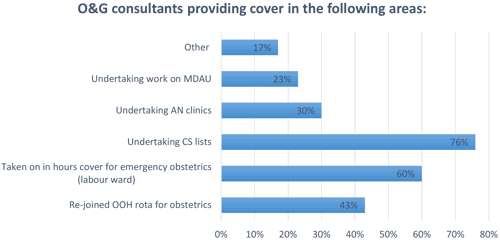
There were noticeable differences between the working patterns of gynaecology consultants and obstetric consultants providing cover during this period. One fifth of all gynaecology consultants providing cover underwent upskilling training in order to provide effective and safe cover to obstetric services. The majority of gynaecology consultants were undertaking caesarean section lists, with a much lower proportion (8%) taking on antenatal clinics. Approximately 50% of gynaecology consultants provided support in emergency obstetrics and re-joined the out of hours’ rota for obstetrics.
4. Staff absences
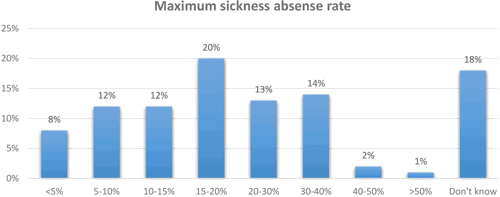
Staff absence due to sickness, caring responsibilities and vulnerability also had a considerable impact on maternity services. As part of the study, respondents were asked to provide a maximum sickness absence rate for O&G staff at their trust/unit. 44% reported between a 5-25% maximum staff absence rate, 29% predicted between 20-50% maximum sickness absence with 18% unable to offer an estimate.
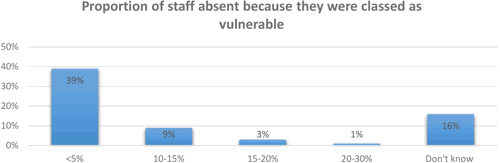
Only 12% of respondents felt that the proportion of staff being absent due to vulnerability was between 10-20%. 39% of trusts fed back that fewer than 5% of their O&G staff fell into this category. Many respondents could not provide this data with any certainty so actual rates may be different from those reported.