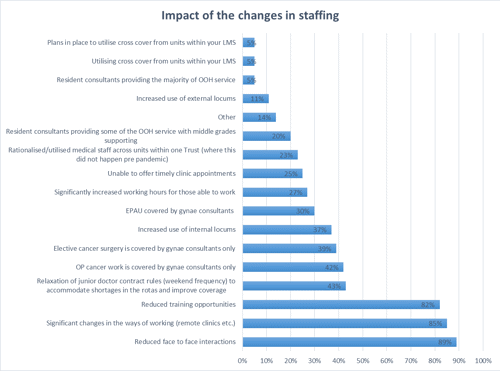
1. Impact of the changes in staffing
There have been several consequences of this redeployment. Overall, 85% of trusts/units reported a significant change in ways of working, with 89% having reduced face-to-face interactions and 82% noting a reduction in training opportunities. Consultants, SAS and middle grade doctors have been placed under increased and unsustainable stress running a core service without a valuable part of the workforce.
A high proportion of trusts experienced a relaxation of junior doctor contract rules in order to accommodate shortages in the rotas and improve coverage. Outpatient cancer and elective cancer surgery was being provided by gynaecology consultants only. There has also been a notable increase in locum use, with a 37% of units who responded reporting an increase in the use of internal locums and 11% reporting an increase in external locum use. This reflects the increased pressure on maternity services.
More than a quarter reported significantly longer hours for those available to work. A similar number stated they were unable to offer timely clinic appointments.
2. Concerns about changes
Over a quarter of survey respondents said they had concerns about the planning and implementation of the medical staff changes at their place of work. Concerns about how the changes were implemented and communicated to staff were by far the most common across all trusts, highlighting the importance of clear and consistent communications when relaying information about staffing changes. Several respondents felt that the redeployment plans lacked efficient planning and transparency and that the changes to their rotas were unnecessary.
The loss of training opportunities was experienced by trusts across the board and in some cases units were not confident that sufficient induction training was provided for staff moving to medical teams. Several respondents were apprehensive about having limited exposure to gynaecology as a direct result of staffing changes and some conveyed that the changes in working patterns resulted in an increased rate of staff sickness at their units.
3. Learning opportunities and positives as a result of the changes
Despite the concerns raised, a large number of survey respondents felt that there were lessons learned and learning opportunities gained through the response to COVID-19. By and large the most collective positive outcome highlighted was the noted increase in staff morale at all levels and sense of comradery amongst teams. Adaptability and flexibility were required to accommodate last minute rota changes due to staff sickness, redeployment, changes in policy and service delivery and several trusts experienced improved team working as a result of these challenges.
In many trusts changes that were in the pipeline, such as telephone triage, outpatient management and MVA provision, were brought forward to meet the service demands. This had a number of positive effects, with some units reporting improved efficiency in their service delivery as senior staff only were doing telephone clinics which resulted in fewer follow-ups. A high proportion of survey respondents also felt that remote clinics have advantages and can be more convenient for some patients with families.
Some trusts reported that there were greater opportunities for reflective practice, leadership, and crisis management, and trainees fed back that their communication skills had improved due to being on the medical rota and having difficult conversations with families during the crisis.
Some consultant gynaecology surgeons felt that they benefited from increased surgical exposure and several junior grade doctors (those who were not redeployed) added that they benefited from increased access to consultants in their work.