Published: July 2017
Please note that this information will be reviewed every 3 years after publication.
This information is for you if you or anyone you know has undergone female genital mutilation or is at risk of having FGM.
It may also be helpful if you are a partner, relative or friend of someone who has been affected by FGM.
FGM can have a lasting physical, mental and psychosexual effect on the girl or woman. It is recognised as a human rights violation and is illegal in the UK.
The information here aims to help you better understand your health and your options for treatment and care. Your healthcare team is there to support you in making decisions that are right for you. They can help by discussing your situation with you and answering your questions.
This information covers:
- What FGM is
- What the different types of FGM are
- The complications of FGM
- What to do if you have had FGM
- What deinfibulation is
- What the options are if you have had FGM and you’re pregnant
- Where you can find further information, care and support
Within this information, we may use the terms ‘woman’ and ‘women’. However, it is not only people who identify as women who may want to access this information. Your care should be personalised, inclusive and sensitive to your needs, whatever your gender identity.
A glossary of medical terms is available at A-Z of medical terms.
Key points
- FGM can have a lasting physical, mental and psychosexual effect on the girl or woman.
- FGM is recognised as a human rights violation and is illegal in the UK.
- There is support available for you if you or anyone you know may be affected by FGM.
- Depending on the degree of cutting (type of FGM), you may be offered a minor operation called deinfibulation to allow intercourse or vaginal birth.
FGM includes all procedures involving the partial or total removal of the external female genitalia or any other injury to female genital organs for nonmedical reasons. It is also sometimes called female circumcision or cutting.
It is illegal to perform FGM in the UK. It is also illegal to arrange (or assist in arranging) for anyone in the UK to be taken abroad for the purpose of FGM. It is recognised as a human rights violation, has no health benefits, and harms girls and women in many ways.
FGM takes place in areas of Africa, Asia and the Middle East, with the highest numbers seen in north-east Africa. Women and girls with FGM now live in countries all over the world, including the UK, particularly among members of some migrant communities.
FGM is usually carried out on young girls from birth onwards but the age and the type of FGM varies between and within different countries. FGM may be performed by untrained individuals who may not use proper antiseptics or anaesthetics.
There are four different types of FGM:
Type 1: Removal of all or part of the clitoris (the small, sensitive and erectile part of the female genitals), sometimes also removing the skin fold (hood) around the clitoris.
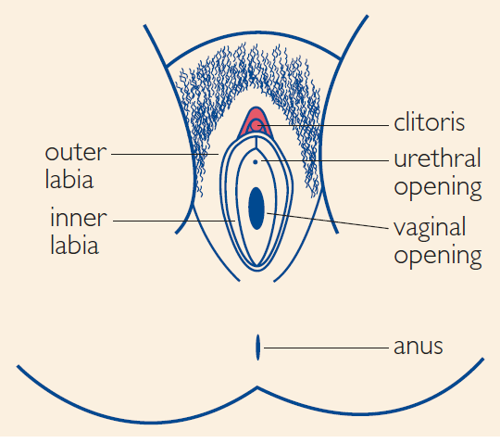
Type 2: Removal of the clitoris with part or all of the inner labia (lips), with or without cutting of the outer labia.
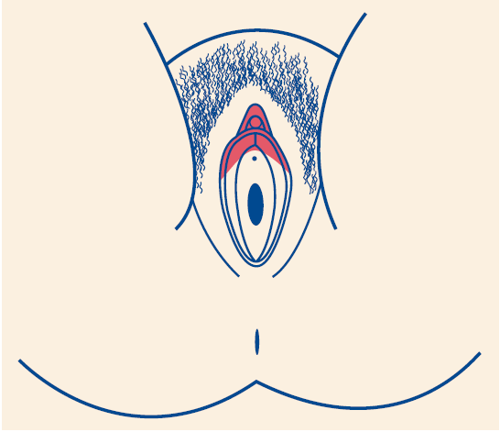
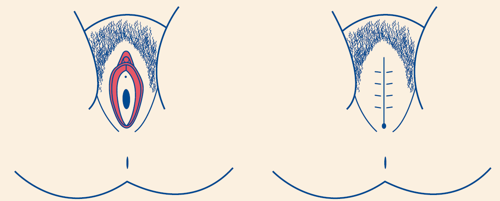
Type 3: Making a covering seal to narrow the vaginal opening by cutting and sewing together the inner and outer labia with or without removal of the clitoris
Type 4: All other harmful procedures to the female genital area for nonmedical reasons, including stretching, pricking, piercing, cutting, scraping and burning
All images courtesy of Royal College of Nursing. Female Genital Mutilation: An RCN Resource for Nursing and Midwifery Practice. Fourth edition. London: RCN; 2019 www.rcn.org.uk/professional-development/publications/pub-007833.
FGM can have a lasting physical, mental and psychosexual effect on you.
You may have a variety of complications which will depend on your individual circumstances.
Soon after the procedure, you may have bleeding, infection, difficulty passing urine or genital swelling. Deaths have also been reported following FGM.
Later on you may develop physical and/or psychological problems. Physical problems may include:
- painful periods
- pain while passing urine
- urinary tract infections
- inability or difficulty in having a vaginal examination and cervical smear
- pain during sex or unable to have sex
- genital scarring
- vaginal narrowing
- reduced sexual pleasure
- problems with childbirth
- increased risk of caesarean section
- increased risk of bleeding after delivery
- higher risk of stillbirth.
Long-term psychological problems may include:
- low self-esteem
- depression
- anxiety
- flashbacks
- post-traumatic stress disorder
- other mental health issues.
Tell your healthcare professional so that you can be offered the care you may need and be referred to the right place for help and support.
FGM is a form of child abuse. If you are under the age of 18 years your healthcare professional is obliged under the law to report FGM to the local safeguarding team and the police, who will deal with the matter sensitively. Please ask questions and let your healthcare professional know if you require support or translation.
Please see the section on further information at the end of this leaflet for details of support organisations.
If you are worried that you may be pressured by your family or community to have FGM, or if you are concerned about any girl who may be at risk of FGM, tell a healthcare professional or contact the National Society for the Prevention of Cruelty to Children (NSPCC) helpline on 0800 028 3550 (free to call and available 24 hours a day). The NSPCC can be contacted anonymously. You can also email the NSPCC at: fgmhelp@nspcc.org.uk
You can also contact ChildLine (www.childline.org.uk) on 0800 1111 (free to call).
Deinfibulation is a minor operation to divide the scar tissue which is narrowing the vaginal opening in type 3 FGM. This is recommended if the vaginal opening is not open enough for you to:
- pass urine normally
- have sex comfortably
- have an internal examination
- have a cervical smear test
- have vaginal surgery
- have a safe vaginal delivery.
Deinfibulation can usually be performed under a local anaesthetic although you may choose to have a spinal or general anaesthetic. If you need to have a deinfibulation procedure you will be given more information about the procedure and have the opportunity to ask any questions.
Antenatal care
You will be referred to the antenatal clinic to be seen by a healthcare professional (obstetrician or midwife) who specialises in caring for women with FGM. You may have an examination to assess the type of FGM you have had and the impact (if any) this may have on your pregnancy and labour.
Depending on the type of your FGM, you may be advised to have deinfibulation (see above). It can be done during pregnancy, in the early stages of labour or at the time of delivery.
It is illegal in the UK to close back (reinfibulate) the area after childbirth. If you have questions about this, you should discuss it with your healthcare professional and you will be offered referral for support and counselling.
Labour
You will be encouraged and supported to have a normal labour. You may be advised to have a deinfibulation as discussed above. If you have a caesarean section for any reason then the option of deinfibulation just after the caesarean section will be discussed with you.
Postnatal
Your healthcare professional will offer you advice on perineal care and hygiene. If your planned deinfibulation was not performed either at or immediately after childbirth, you will be given a gynaecology outpatient or FGM clinic appointment so that you can consider having deinfibulation before planning any future pregnancies. It is important for you to consider how you can protect your daughter(s) and other female children from FGM. Your healthcare team will discuss this with you.
Whether you are pregnant or not, you can get information and support from any healthcare professional. You can also find details of specialist FGM clinics and services at: www.nhs.uk/fgm.
You may be offered referral for psychological support. If this is something you feel that you would like, ask your healthcare professional who can arrange an appropriate referral.
About intimate examinations
The nature of gynaecological and obstetric care means that intimate examinations are often necessary.
We understand that for some people, particularly those who may have anxiety or who have experienced trauma, physical or sexual abuse, such examinations can be very difficult.
If you feel uncomfortable, anxious or distressed at any time before, during, or after an examination, please let your healthcare professionals know.
If you find this difficult to talk about, you may communicate your feelings in writing.
Your healthcare professionals are there to help and they can offer alternative options and support for you.
Remember that you can always ask them to stop at any time and that you are entitled to ask for a chaperone to be present. You can also bring a friend or relative if you wish.
Further information
GOV.UK – Female Genital Mutilation: The Facts which is part of a larger collection of information on FGM
GOV.UK – Multi-agency Statutory Guidance on Female Genital Mutilation
GOV.UK – Statement Opposing Female Genital Mutilation (‘health passport’)
GOV.UK – Female Genital Mutilation (FGM): Mandatory Reporting Duty
Royal College of Nursing – Female Genital Mutilation: An RCN Resource for Nursing and Midwifery Practice
Daughters of Eve – What is Female Genital Mutilation (FGM)?
Brook – Female Genital Mutilation (FGM)
Forward – FGM
National Society for the Prevention of Cruelty to Children (NSPCC):
The NSPCC (www.nspcc.org.uk) has a dedicated FGM helpline that provides information and advice for families and frontline professionals at 0800 028 3550 (free to call).
If you are asked to make a choice, you may have lots of questions that you want to ask. You may also want to talk over your options with your family or friends. It can help to write a list of the questions you want answered and take it to your appointment.
Ask 3 Questions
To begin with, try to make sure you get the answers to 3 key questions, if you are asked to make a choice about your healthcare:
- What are my options?
- What are the pros and cons of each option for me?
- How do I get support to help me make a decision that is right for me?
*Ask 3 Questions is based on Shepherd et al. Three questions that patients can ask to improve the quality of information physicians give about treatment options: A cross-over trial. Patient Education and Counselling, 2011;84:379-85
Sources and acknowledgements
This information has been developed by the RCOG Patient Information Committee. It is based on the RCOG Green-top Clinical Guideline No. 53 Female Genital Mutilation and its Management. The guideline contains a full list of the sources of evidence we have used.
This information was reviewed before publication by a number of organisations dedicated to working with women affected by FGM and by women themselves across the UK who, either directly or indirectly, have experience of FGM. The information was also reviewed by the RCOG Women’s Network and by the RCOG Women’s Voices Involvement Panel.
