Repair of third- and fourth-degree tears, how to care for stitches, and what to expect when healing
For some women, a tear may be deeper and extend to the muscle that controls the anus (the anal sphincter).
Third- or fourth-degree tears, also known as an obstetric anal sphincter injury (OASI), can occur in 6 out of 100 births (6%) for first time mothers and less than 2 in 100 births (2%) of births for women who have had a vaginal birth before.
A rectal buttonhole is a rare injury that occurs when the anal sphincter does not tear, but there is a hole between the back passage and the vagina. This means that wind and faeces may be passed through the vagina instead of via the anus.
Repair of third- and fourth-degree tears
If you have sustained a third-degree, fourth-degree or rectal buttonhole, you will be transferred to an operating theatre as soon as possible after your baby is born.
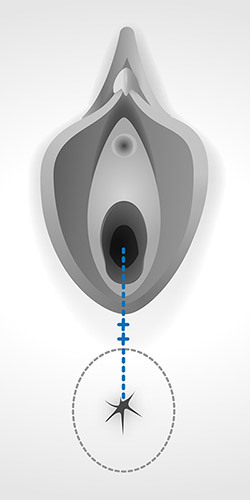
You will be given spinal or epidural anaesthesia so that you have good pain relief whilst your muscles are repaired. You will have stitches between your vagina and anus (see diagram) and also underneath your skin. The stitches will eventually all dissolve (soften and fall out).
You may need a drip in your arm to give you fluids until you feel ready to eat and drink. You are likely to need a catheter (tube) in your bladder to drain your urine. This is usually kept in until you are able to walk to the toilet.
Following the repair, you will be given antibiotics and pain relief.
Medications should not affect your ability to breastfeed.
How do I prevent infection?
Good hygiene is important. Use only water to keep the area clean.
Wash or shower at least once a day and change your sanitary pads regularly.
Wash your hands both before and after you go to the toilet, or change your sanitary pads.
This will reduce the risk of infection in the stitches.
I think my wound is infected, how do I know?
Signs of infection include:
- Red, swollen skin around the stitches
- Discharge, or pus from the wound
- Increase in pain, or tenderness at the wound
- A smell that isn’t normal for you
- Fever
If you have any of these signs or symptoms you should see your healthcare professional. You may require antibiotics to help it heal, or if you have been given antibiotics already you may need your medication reviewed.
Should I feel pain after the wound has healed?
After having any tear, it is normal to feel pain or soreness for 2-3 weeks after giving birth, particularly when walking or sitting.
The stitches can irritate as healing takes place but this is normal.
Passing urine can cause stinging. Pouring body-temperature water over the area when urinating can help.
The skin part of the wound usually heals within a few weeks of birth, and after that you should feel much less raw and tender.
Should my scar tissue be uncomfortable?
It may feel uncomfortable at first, particularly for 2-4 weeks after giving birth.
If the scar tissue continues to be uncomfortable you should seek medical attention.
If I get constipated, will the tear open up again?
Opening your bowels should not affect your stitches. After your third- or fourth-degree tear is repaired, you will be given some laxatives for the first few days, so that you don't get constipated and don’t need to strain to open your bowels.
Sometimes, the laxatives work so well that you may struggle to get to the toilet in time. This should improve and settle over the first few days.
It is important to eat well and drink plenty of water to help avoid constipation.
You should drink at least 2 litres of water every day and eat a healthy balanced diet (for instance: fruit, vegetables, cereals, wholemeal bread and pasta).
What will help to open my bowels?
It can be helpful to put your feet on a footstool to raise your knees above your hips while sitting on the toilet (see image). This helps straighten out the bowels.
Try to relax and rest your elbows on your knees. Do not strain, as this weakens the pelvic floor.
Bulge out your tummy by taking big abdominal breathes, this will help expel your faeces without straining. Straining weakens your pelvic floor and anal sphincter muscles and you want to avoid this.
Gently push down from your back passage rather than holding your breath.
Most importantly, take your time and do not rush.

How can I improve my bowel control?
Don't delay if you have the urge to empty your bowels.
It is important to do pelvic floor exercises as soon as you can after birth.
Gentle pelvic floor exercises strengthen the muscles around the vagina and the anus, which should help improve bowel control.
You may feel that initially after childbirth, your pelvic floor muscles are not very strong.
You may also feel that you have difficulties working with your pelvic floor and that you have very little sensation.
This usually improves with time and the more you are able to work your pelvic floor muscles, the quicker the recovery will be.
What is anal incontinence?
Anal (or faecal) incontinence is when you have problems controlling your bowels.
Symptoms include sudden, uncontrollable urges to open your bowels, or not being to control passing wind.
You may also soil yourself or leak faeces.
Don't be embarrassed about talking to a healthcare professional if you have these symptoms as support and treatment is available for you.
Will I get anal incontinence in the future?
Most women who have a third- or fourth-degree tear heal completely and have no lasting complications.
However, a small number of women will experience difficulty in controlling their bowels or passing wind.
People who experience these symptoms should receive appropriate care, which may include physiotherapy or surgery. Physiotherapy will include teaching you how to correctly squeeze and strengthen your anal sphincter muscles to help reduce incontinence.
What level of activity should I do?
Everyone's experience will be slightly different, and what you view as normal daily activities will differ.
For 4-6 weeks, you should avoid strain or pressure on the anus, and avoid high impact exercise or heavy lifting.
After this, you can gradually increase your general activity.
Looking after a newborn baby and recovering from a third- or fourth-degree tear can be hard. Support from family and friends can help you whilst your body gradually adjusts and gets better.
When can I have sex again?
It's common to be worried by the thought of resuming sexual intercourse after having given birth, particularly if you have experienced a third- or fourth-degree tear.
Once your stitches have healed and bleeding has stopped, you can have sex again when it feels right for you.
Prior to commencing intercourse, you should consider a suitable method of contraception. It is possible to get pregnant very soon after giving birth.
Perineal massage, either on your own or with your partner, may help you feel more comfortable before you begin having sex again.
Sometimes, women who have recently had a baby may notice the vagina is drier than usual, this can be the case particularly if you are breastfeeding.
You may wish to use an appropriate lubricant the first few times you have intercourse (if you are using condoms you should use a water-soluble gel).
Sex may be a little uncomfortable and feel different at first, but the discomfort should not persist.
Chatting with your partner about sex and any anxieties either of you may have and choosing a time when you both feel relaxed can help.
What will happen if I have another baby?
Many women go on to have a straightforward vaginal birth after a third- or fourth-degree tear.
If you continue to experience symptoms from the third- or fourth-degree tear, you may wish to consider a planned caesarean section.
You will be able to discuss your options for future births at your follow-up appointment or early in your next pregnancy.
Your individual circumstances and preferences will always be taken into account so that you can make a decision that is right for you.
Post-traumatic stress disorder
Having a third- or fourth-degree tear can be very distressing and disturbing for women, their partners and their families.
For some women who experience any birth trauma there is a risk of post-trauma stress disorder (PTSD).
Symptoms include flashbacks, heightened anxiety, low mood or isolation.
You may find it hard to bond with your baby.
PTSD can develop immediately after the event, or can occur several weeks, months or years later.
If you, or your partner, experience signs of PTSD, contact your healthcare professional as help is available for you.
Will I have any follow-on appointments?
You will usually be offered an appointment with a healthcare professional approximately 6 weeks after you had your baby to make sure that you are recovering well.
At that appointment, you will be able to discuss any concerns and ask any questions you may have about the birth of your baby and any of your symptoms or concerns about future pregnancies.
You may be given an appointment with a physiotherapist to help you strengthen your pelvic floor muscles.
When should I contact a healthcare professional?
- If you are concerned about your stitches in any way (for instance they are painful, swollen, smelly).
- If you are worried that repaired tear has opened.
- If you experience signs of infection (e.g. fever).
- If you are experiencing any signs of anal incontinence.
- If you pass faeces through your vagina.
- If you experience pain during sexual intercourse.
- If you experience signs of PTSD.
- If you have any concerns.
Organisations offering information and support
The MASIC Foundation
https://masic.org.uk
Birth Trauma Association
www.birthtraumaassociation.org.uk
Bladder and Bowel Foundation
www.bladderandbowel.org
Pelvic, Obstetric & Gynaecological Physiotherapy (POGP)
https://thepogp.co.uk
Further reading
RCOG patient informational leaflet
Third- or fourth-degree tear during childbirth
Sex and contraception after childbirth
https://www.nhs.uk/conditions/pregnancy-and-baby/sex-contraception-after-birth/
Caring for yourself after an episiotomy or tear during childbirth
https://www.nct.org.uk/labour-birth/you-after-birth/episiotomy-during-childbirth
Post-traumatic stress disorder
https://www.nhs.uk/conditions/post-traumatic-stress-disorder-ptsd/
