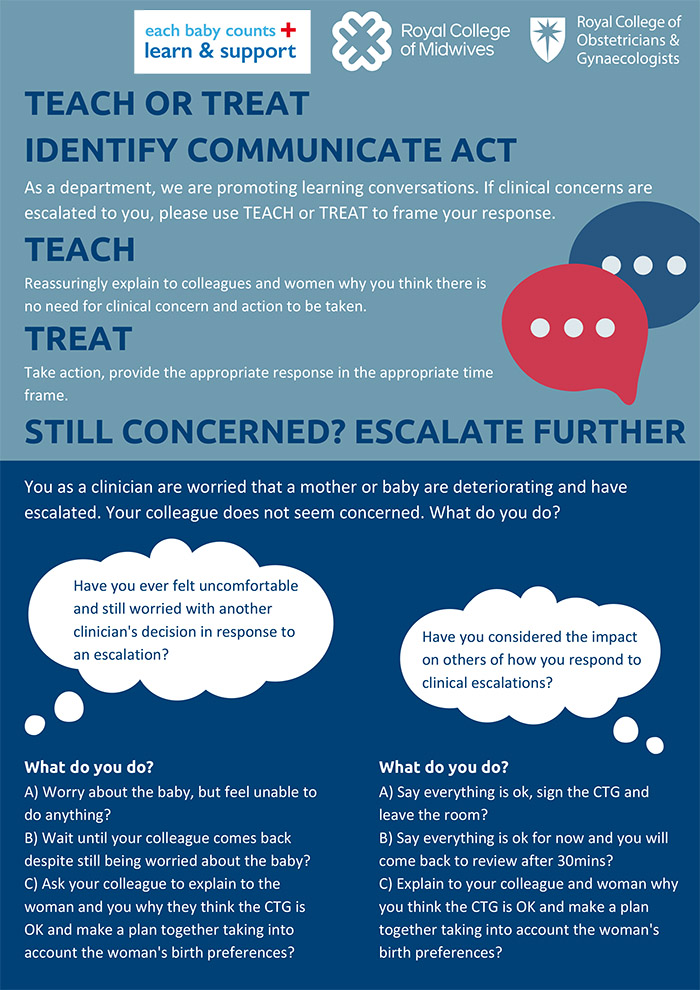
Teach or Treat is a communication strategy which encourages a discussion about the clinical situation being escalated: initiating a kind, quick and respectful response.
It is both about exploring ways to escalate and reducing hierarchical decision making. It promotes a collaborative understanding about the unravelling clinical situation, learning and understanding from everyone’s perspectives, and encourages respect for the opinion of others.
The concept is most elegantly described using the following scenario. It is common in intrapartum care for a case midwife to escalate concerns about a CTG (cardiotocograph) to another member of staff. Interpretation of CTGs is complex, and needs to be contextualised with both the progress and stage of labour, and the clinical risk factors for the mother and baby. It is not uncommon for a case midwife to have concerns over fetal wellbeing due to a combination of CTG changes and risk factors, but for another, rushed member of staff to make a cursory assessment and potentially dismiss their concerns (and in some cases, the woman as well). If the other member of staff is higher in the leadership hierarchy (senior midwife or obstetrician) it can sometimes leave the case midwife with both ongoing concerns, or a fear of escalating again. This in turn can lead to mistakes – either because the person being escalated to made an incorrect assessment, or because future escalations don’t happen in a timely fashion due to fear of being dismissed.
“Teach or Treat” therefore encourages staff to have respectful, learning conversations during escalation. So, in the CTG scenario, the person being escalated to “teaches” the other member of staff and the woman about their interpretation of current fetal wellbeing. This has 2 benefits. Firstly, if they have missed crucial information or made an incorrect assessment, it provides an additional opportunity to have a more thorough comprehension of the clinical scenario. Secondly, if their holistic assessment has taken everything into account and there is good evidence of fetal wellbeing, it provides a learning opportunity for the other, potentially more junior member of staff, as well as empowering the woman about her care.
If both members of staff are in agreement about the holistic assessment of fetal wellbeing and action is recommended, then this is the “treat” element. A respectful conversation between the staff members and the woman needs to take place, taking into account the woman’s views and preferences. If used effectively and within our guidance, ‘Teach or Treat’ can also empower individuals to escalate further if required – if disagreement remains between staff members then a third opinion should be sought.
Overall, it provides a chance to obtain extra detail about a situation rather than just receiving a short answer, reducing clichéd or jargon biased responses. It can be reassuring for the women being cared for too, they can feel reassured that there is a framework for communication. It must be emphasised that they should be included in the conversation at the appropriate time if they are witnessing it. It is a clear concept - teach or treat, in order that conversations become meaningful and precise and most importantly, effective.
What does Teach or Treat aim to do?
- Promote respectful conversations between staff members so that junior members of the team are not afraid to be unsure, be wrong, or escalate concerns.
- Promote shared understanding of a clinical situations from different clinicians’ perspectives
- Put the woman at the heart of the decision making and information giving
- Identify when escalation has taken place
- Promote a flattened hierarchy, a culture of learning and of mutual respect
- Empower all members of the team to respectfully challenge if they think another member may be making a mistake
When is Teach or Treat used?
- When implemented in units around the country, it was most widely used when interpreting CTGs. However, it can be used in any clinical situation.
- On ward rounds
- When performing “fresh eyes” if there is disagreement between the two clinicians
- When escalating clinical concerns
- In CTG / intrapartum care teaching
What do clinicians say about it?
- Widely accepted as a positive intervention “it makes you really think about your behaviours and actions, and promotes you to have better conversations”
- It improves multi-disciplinary relationships
- It makes staff feel safe
- It flattens hierarchies and empowers junior staff
- It promotes staff to reflect on their decisions and create collaborative care plans
What do women think?
- Women who witnessed the conversations received reassurance and better understandings of their own situation, whilst describing the conversations as respectful.
What are the potential barriers?
- Staff members reported they were more likely to use it in the daytime than overnight, or during periods of high activity. They reflected though that this is often the time it’s needed most.
- Some staff are naturally better at communicating than others – there was therefore some resistance in individuals.
- It needs to be emphasised that it is a way of promoting better conversations – some people dislike using terminology such as “teach or treat”.
- On the whole, it was well adopted my midwives and junior medical staff. Getting buy in from some consultant obstetricians who can model the behaviours is therefore highly advised when implementing this intervention.
Key implementation strategies
- Send introductory emails, place posters around the unit
- Discuss it at all handovers, huddles until embedded
- Shop floor champions – and engage the early adopters
- Be prepared to receive feedback – acknowledge that change can be hard
- Use it in training sessions – particularly CTG / intrapartum care teaching
- Disseminate it to the whole MDT so that it becomes normalised practice in your unit
- Celebrate successes