The Each Baby Counts Learn & Support programme has been focused around our Logic Model
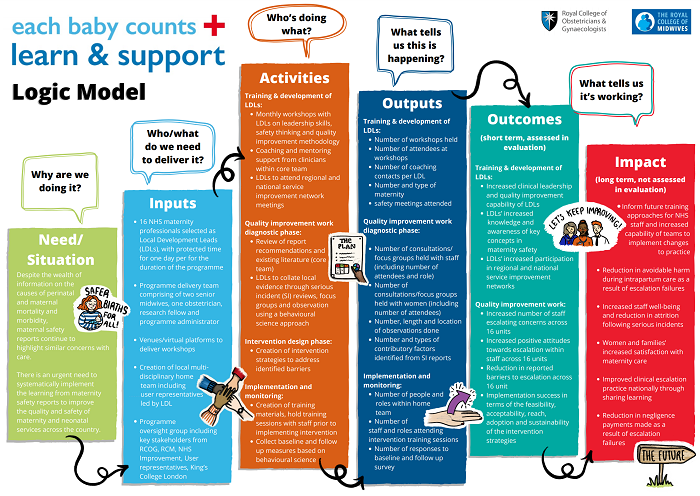
Our logic model consists of six sections:
Why are we doing it?
Despite the wealth of information on the causes of perinatal and maternal mortality and morbidity, maternal safety reports continue to highlight similar concerns with care.
There is an urgent need to systematically implement the learning from maternity safety reports to improve the quality and safety of maternity and neonatal services across the country.
Who/what do we need to deliver it?
16 NHS maternity professionals selected as Local Development Leads (LDLs), with protected time for one day per for the duration of the programme
Programme delivery team comprising of two senior midwives, one obstetrician, research fellow and programme administrator
Venues/virtual platforms to deliver workshops
Creation of local multidisciplinary home including user representatives led by LDL
Programme oversight group including key stakeholders from RCOG, RCM, NHS Improvement, user representatives, King’s College London
Who's doing what?
Training & development of LDLs:
- Monthly workshops with LDLs on leadership skills, safety thinking and quality improvement methodology
- Coaching and mentoring support from clinicians within core team
- LDLs to attend regional and national service improvement network meetings
Quality improvement work diagnostic phase:
- Review of report recommendations and existing literature (core team)
- LDLs to collate local evidence through serious incident (SI) reviews, focus groups and observation using a behavioural science approach
Intervention design phase:
- Creation of intervention strategies to address identified barriers
Implementation and monitoring:
- Creation of training materials, hold training sessions with staff prior to implementing intervention
- Collect baseline and follow up measures based on behavioural science
What tells us this is happening?
Training & development of LDLs:
- Number of workshops held
- Number of attendees at workshops
- Number of coaching contacts per LDL
- Number and type of maternity safety meetings attended
Quality improvement work diagnostic phase:
- Number of consultations/ focus groups held with staff (including number of attendees and role)
- Number of consultations/focus groups held with women (including number of attendees)
- Number, length and location of observations done
- Number and types of contributory factors identified from SI reports
Implementation and monitoring:
- Number of people and roles within home team
- Number of staff and roles attending intervention training sessions
- Number of responses to baseline and follow up survey
What tells us it's working? Short-term, assessed in evaluation
Training & development of LDLs:
- Increased clinical leadership and quality improvement capability of LDLs
- LDLs’ increased knowledge and awareness of key concepts in maternity safety
- LDLs’ increased participation in regional and national service improvement networks
Quality Improvement work:
- Increased number of staff escalating concerns across 16 units
- Increased positive attitudes towards escalation within staff across 16 units
- Reduction in reported barriers to escalation across 16 units
- Implementation success in terms of the feasibility, acceptability, reach, adoption and sustainability of the intervention strategies
What tells us it's working? Long-term, not assessed in evaluation
- Inform future training approaches for NHS staff and increased capability of teams to implement changes to practice
- Reduction in avoidable harm during intrapartum care as a result of escalation failures
- Increased staff well-being and reduction in attrition following serious incidents
- Women and families’ increased satisfaction with maternity care
- Improved clinical escalation practice nationally through sharing learning
- Reduction in negligence payments made as a result of escalation failures
