Teams delivering intrapartum care are large, complex and involve many professional and hierarchical roles.
It is not uncommon to be unfamiliar with some members of the team in any given shift. However, optimal communication and clinical escalation, particularly in rapidly emerging time critical situations relies on effective teamwork and leadership. It also requires high levels of trust, an understanding of each other’s job roles, and a shared mental model of the team’s workload.
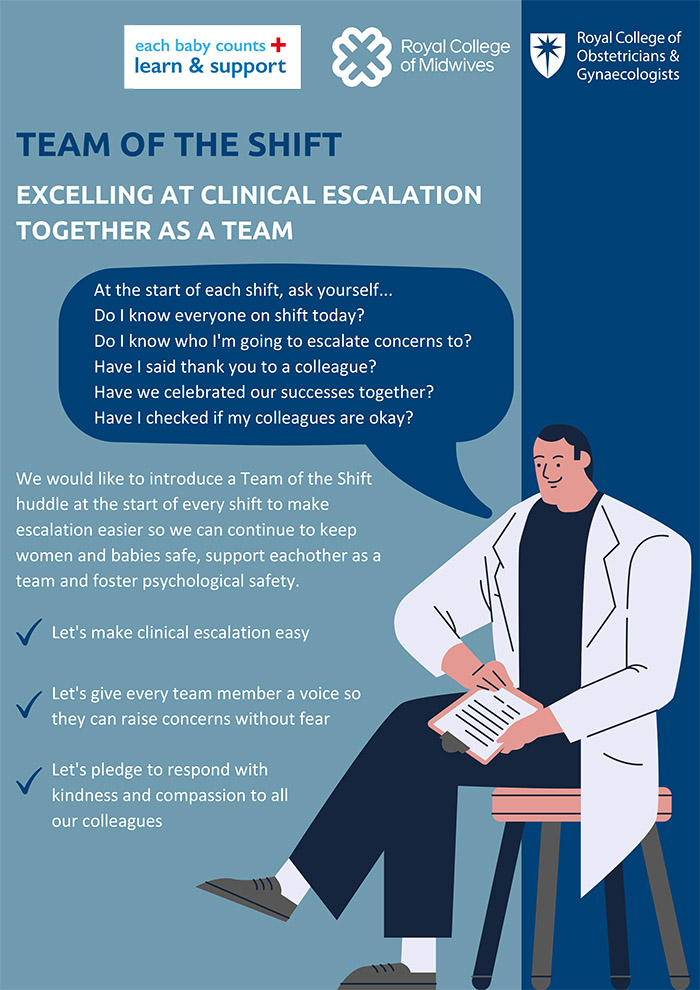
Unlike other parts of medicine there was no existing current guidance on best practice in establishing a team of the shift in maternity care. The team of the shift intervention was therefore designed to standardise a huddle at the start of every shift, prior to clinical handover in order to promote excellence in teamwork.
The gold standard would be for all members of the multidisciplinary team to be present, (including representatives from neonatal and theatre staff), but differing shift patterns between staff groups often prevent this. In addition, many units lack the physical infrastructure to accommodate such a large group of people, although this is increasingly overcome using technology.
What does Team of the Shift aim to do?
- Identify all the staff on shift that day, including job role and length of shift
- Identify the team leaders, including those who will be escalated to
- Flatten hierarchies by giving everyone a voice and encouraging first name introductions
- Support staff by creating psychological safety, encouraging them to raise concerns and speak up
- Identify anyone in the team who may need additional support that day
- Identify learning needs for trainees and students
- Create a positive workplace culture by thanking staff and celebrating successes
- Foster a culture of kindness and civility
- Eliminate cultures of criticism, including “toxic handovers”
- Foster a sense of teamwork, mutual respect, and create a shared mental model of the team’s workload, priorities, and potential challenges that shift
When is Team of the Shift Used?
- At the start of every shift, particularly in complex intrapartum care areas
- Prior to clinical handover
What did clinicians say about it?
- Easy to implement by some suggested and sustain
- It opens discussions around creating psychological safety “learning to make time to introduce people to one another and talk about escalation to in turn creates safer shifts”.
- Impacts positively on staff during a time of high workload and low morale
- Makes escalation more efficient
- Builds trust, respect, and a sense of unity.
- Identifies individual needs within the team to plan areas of support as well as providing a positive and supportive way to start a shift.
- Empowers junior staff
- Introductions were noted as particularly helpful to avoid confusion and improve safety on the unit.
What are the potential barriers?
- Different shift start times
- Times of high acuity
Implementation strategy
- Send out a version of these email templates:
- Engage your shift leaders – in particular, band 7 midwives / senior obstetricians. Let them know it’s coming
- Put up these posters in your handover area:
- Hand out the business cards containing this to all staff:
- Do you know everyone on your shift today?
- Do you know who you're going to escalate concerns to during the shift?
- Have you said thank you to a colleague?
- Have you celebrated your successes together?
- Have you made sure your colleagues are okay at the beginning and end of each shift?
- Consider other change ideas to promote a positive culture – eg thank you cards, positive feedback disseminated by risk management team
- Consider adopting other strategies to help identify key roles and staff names in emergencies – eg different coloured scrubs, lanyards, scrub hats with names and roles on.